Lyme Disease: Neurological Lyme and Neuropathy
Aug 26, 2025Lyme Disease Treatment: Neurological Lyme (Neuro Lyme) and Neuropathy
Hello — I’m Dr. Stanley Lang, M.D. this article I’ll walk you through an overview of what I’ve seen and learned about neurological Lyme disease (neuro Lyme), how it can present as neuropathy and many other neurological problems, and what that means for diagnosis and long‑term management.

This piece is based on material I shared in a video with Hope For Good Health and expands on the clinical patterns and practical takeaways I’ve observed over the years.
Can neuropathy be a symptom of chronic Lyme disease?
Short answer: Yes. Neuropathy — tingling, numbness, burning sensations or other abnormal sensations in the hands, feet, arms or legs — can certainly be caused by chronic Lyme disease. In fact, almost any neurological symptom can be associated with this infection.
“Chronic Lyme disease can mimic many different neurological conditions.”
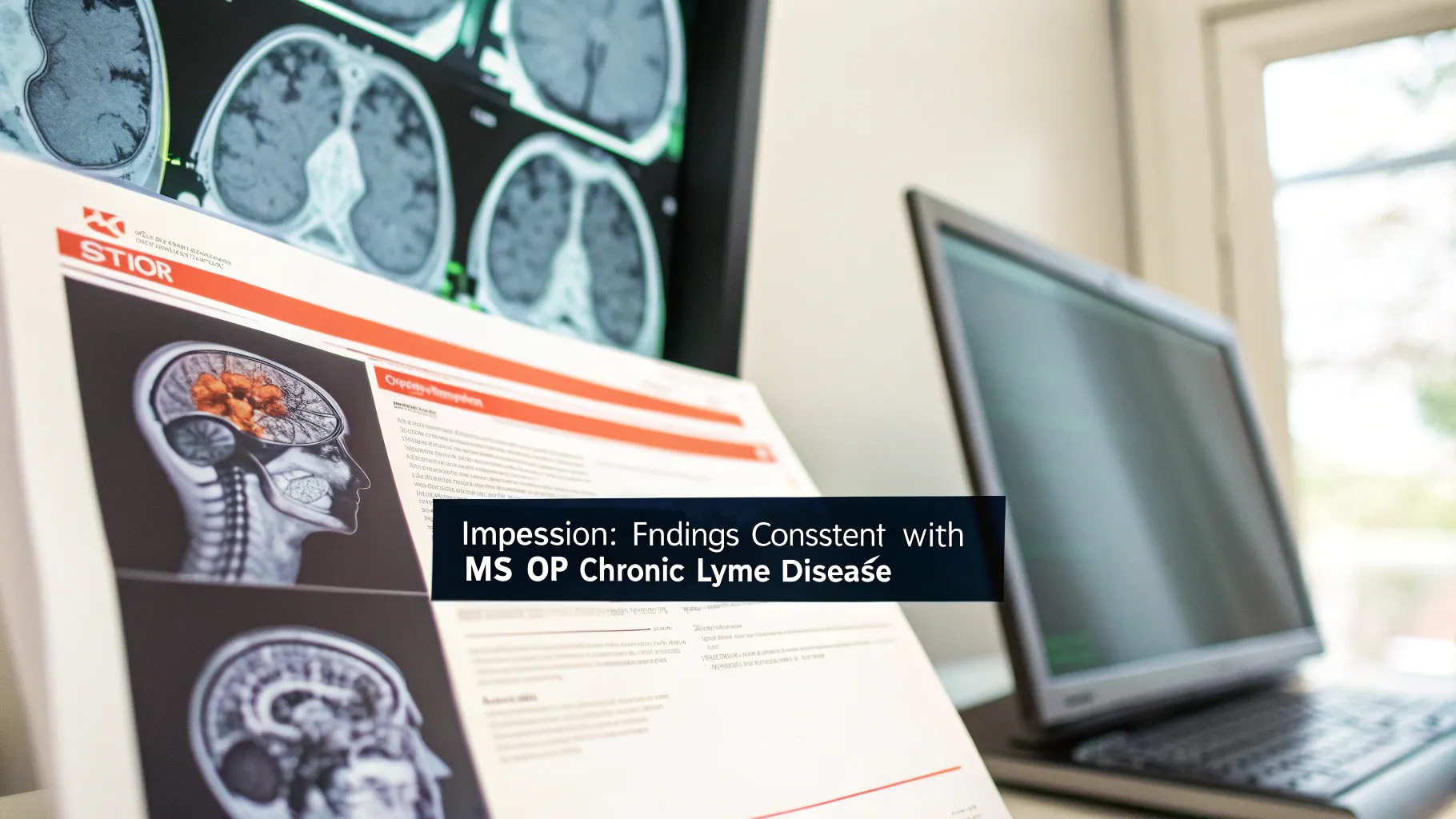
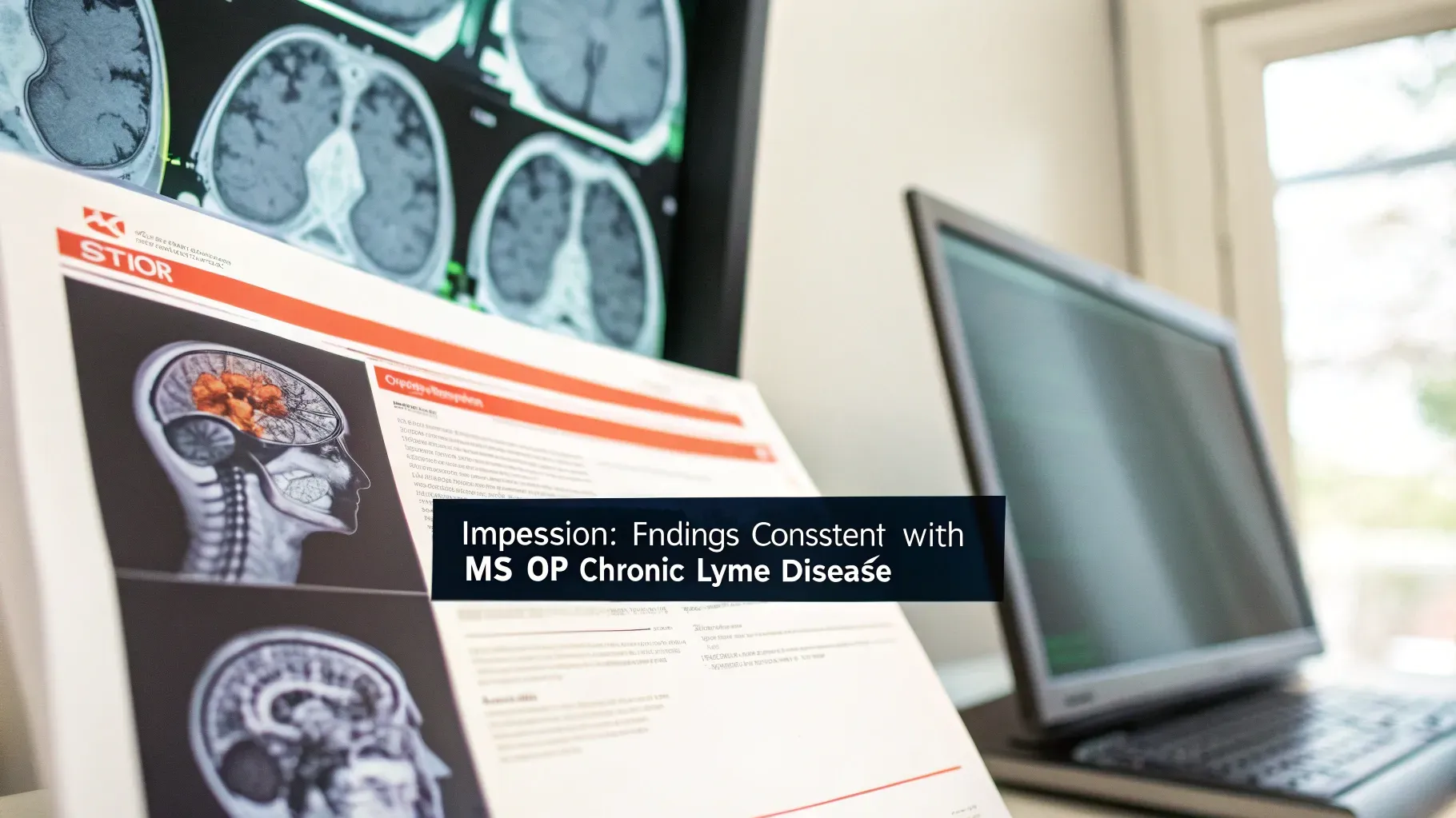
Radiologists sometimes list “consistent with MS or chronic Lyme disease” on MRI reports because neuro Lyme can look very similar to other neurological disorders. That mimicry can make diagnosis challenging, especially when Lyme isn’t suspected early on.
Real cases: how neuro Lyme can present
Over the years I’ve seen a wide range of neurological presentations linked to Lyme infection. A few examples:
- Profound memory loss: One memorable patient was a man under 25 who developed severe memory problems — nearly indistinguishable from advanced dementia — to the point he couldn’t find his way to work. After testing and treating for Lyme, his memory improved rapidly, and he fully recovered. He later relapsed with the same symptom complex on two separate occasions years apart, which is a pattern I’ve seen before.
- Peripheral neuropathy: Tingling, burning, numbness especially in the feet (and sometimes hands) that can be persistent and disruptive.
- Tinnitus (ringing in the ears): I’ve treated patients with severe, recurring tinnitus that improved markedly when we addressed Lyme infection.
- Mimics of other diseases: Symptoms can resemble multiple sclerosis, chronic fatigue syndromes, cognitive disorders, and other neurological illnesses.
Patterns that provide diagnostic clues
Two practical patterns I look for clinically:
- Recurrence with similar symptoms: When a patient recovers and then relapses, the relapse often reproduces the patient’s original symptom set. That repetition is a helpful clue pointing toward chronic Lyme.
- Variable neurological complaints: Because Lyme can affect many parts of the nervous system, you can see very different complaints in different people — from cognitive loss to neuropathic pain to ear symptoms.
“Virtually anything in the neurological system can be infected with this organism.”
Why neurological infections are hard to clear
The central and peripheral nervous systems are relatively protected environments. Once Lyme organisms or their effects reach nervous tissue, they can be difficult to eradicate completely.

That does not mean we’re helpless — it means treatment and long‑term strategies often need to be comprehensive, targeted, and sustained.
It’s also important to note that antibiotics alone are not always sufficient. Many clinicians and patients find that a multimodal approach — addressing immune support, inflammation, co‑infections, and neural repair in addition to antimicrobial therapy — is required for durable improvement.
Common neurological symptoms of chronic Lyme disease
- Memory loss, brain fog, and cognitive difficulties
- Peripheral neuropathy: tingling, numbness, burning in extremities
- Tinnitus (ringing in the ears)
- Headaches and migrainous patterns
- Balance problems or dizziness
- Mood changes, anxiety, or depression linked to neurological dysfunction
Practical tips — what to do if you suspect neuro Lyme
- See a clinician experienced with Lyme and neurological presentations. Early, accurate evaluation matters.
- Consider a full assessment: history (including past tick exposures), focused neurological exam, appropriate laboratory testing and imaging when indicated.
- Be aware of recurrence patterns. If symptoms resolve and later return with the same features, that pattern is a helpful diagnostic clue.
- Expect a multimodal treatment plan. Managing neuro Lyme often involves more than a single antibiotic course — immune support, anti‑inflammatory strategies, symptom management, and rehabilitation may all play roles.
- Monitor and follow up long term. Because nervous‑system involvement can relapse, ongoing monitoring and maintenance strategies are frequently needed to keep symptoms suppressed.
Where I’m going next — suppression and long‑term management

There are ways to keep neuro Lyme suppressed so that people can regain function and maintain it. In future discussions I’ll outline the critical steps I use in long‑term management, including natural and integrative strategies that complement antimicrobial therapy. These steps are not one‑size‑fits‑all — they must be tailored — but when done correctly they can make a big difference.
Final thoughts
Neurological Lyme disease is a serious form of chronic Lyme that can masquerade as many other neurologic conditions. If you or someone you care for has unexplained cognitive decline, neuropathy, tinnitus, or other neurological symptoms — especially with a relapsing pattern — consider evaluation for Lyme disease by a clinician familiar with its neurological presentations.
Thank you for reading. I shared these observations and cases on the Hope For Good Health channel, and I’ll continue to provide practical guidance on diagnosis, treatment strategies, and ways to suppress neuro Lyme effectively. God bless and take care.
Stanley Lang, M.D.
Click Here to Access Your First Trial of StemWave Pain management
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
